What is Clinical Validation of a Blood Pressure Monitor?
Clinical validation is a formal study comparing the accuracy of a blood pressure monitor relative to the measurement of an observer using a mercury sphygmomanometer and stethoscope on a patient. Under this scenario, the trained healthcare practitioner uses the above tools in a controlled environment, with a prepared patient, and compares that reading to the blood pressure device in question.
Validation studies are not created equal
Unfortunately, the phrase “clinically validated” has become as ubiquitous as other marketing claims because the process of clinical validation is not always followed to its fullest measure – or for each applicable product line. Healthcare professional need to understand the process of clinical validation in order to assess manufacturer claims to ensure that they are using and recommending blood pressure monitors that proven accurate.
To that end, clinical validation is comprised of a three major components:
- Utilization of modern protocols
- Independent verification of accuracy
- Publication in a peer-reviewed journal
Educating Patients is Key for Accurate Home Measurements
The first part is educating patients to obtain a reliable, accurate home blood pressure monitor.
- Make sure your patients understand that their home monitor should be clinically validated.
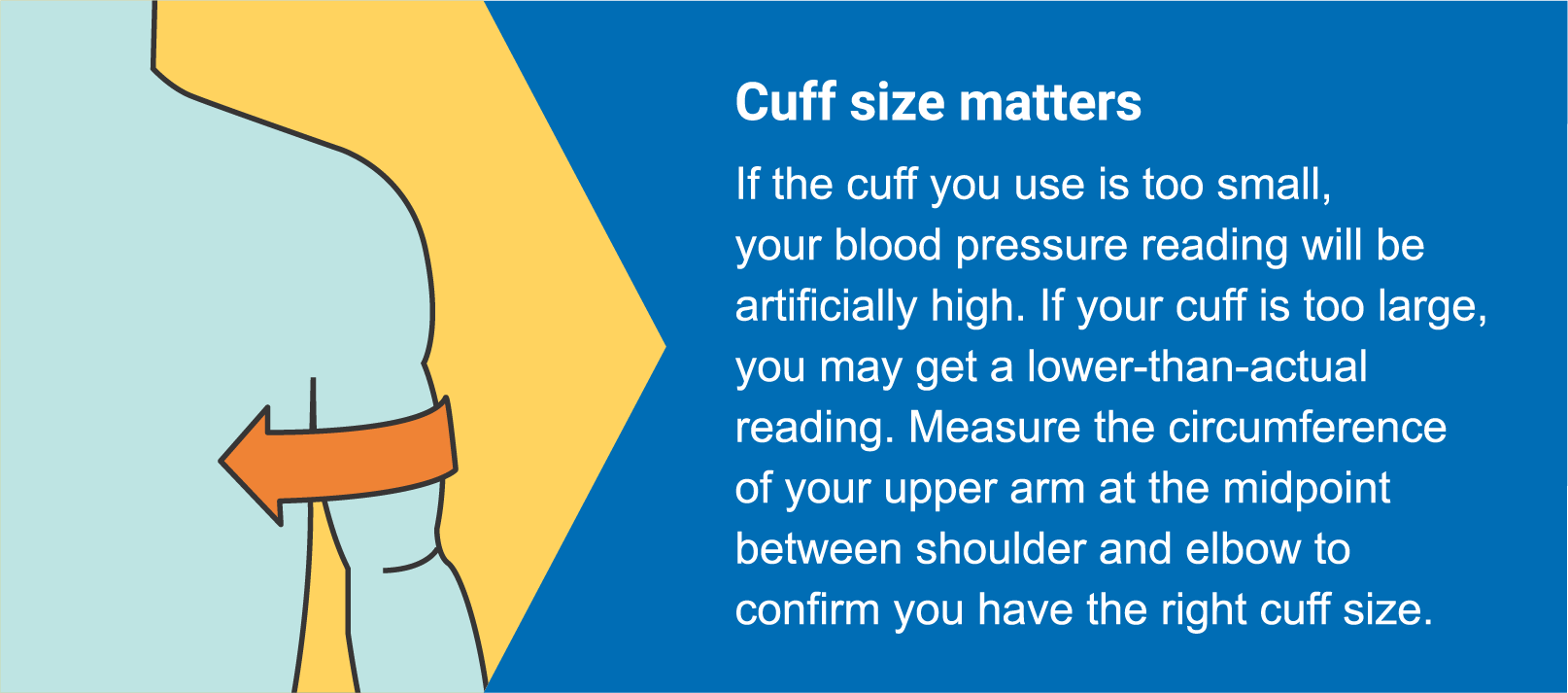
- Instruct patients to measure their arm to make sure they have an appropriate size cuff.
The second part of education is using proper technique.
30 minutes before you take your measurement, do not exercise, do not drink coffee, caffeinated soda, or alcohol, and do not smoke. Sit quietly for 5-10 minutes to relax.
- Sit on a chair with your back straight, your legs uncrossed, and your feet flat on the floor.
- Secure the cuff snugly cuff on your arm or wrist. Rest your arm on a table for support and make sure the cuff is at heart level.
- Press start. During your measurement, do not talk or move.